COVID Times Two
Run into a rebound? Researchers seek to evaluate the virtues of anti-COVID meds like Paxlovid
Here’s the story: You catch COVID, or, more accurately, COVID catches you.
Luckily, it’s happening now rather than two years ago when nobody knew what the virus was or how to treat it.
Armed with the latest data, you head for your doctor’s office to pick up Paxlovid. You take your pills as directed and hooray! In just five days your symptoms are gone and your virus levels are down.
But not for long. Like Anthony Fauci and Jill Biden, a few days later you test positive again. You’re not alone. As one patient who’s run out of patience puts it, “Virtually everyone I know, including me, who’s taken Paxlovid has run into a rebound even worse than the original bout.” As a result, some people who have so far escaped even one round of COVID pinky-swear not to take Paxlovid if they do get sick.
Does that make medical sense? Probably not, because the culprit may not be an ineffective medicine but the tricky little beast called SARS-CoV-2, short for Severe Acute Respiratory Syndrome Coronavirus 2.
The ACTIV-2/A5401 Study Team is a group of researchers from Harvard, UCLA, the University of North Carolina and the University of Washington seeking to evaluate the virtues of anti-COVID meds like Paxlovid.
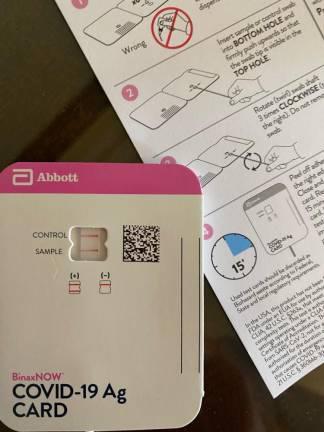
After securing the backing of the National Institutes of Health, they enrolled 568 COVID positive patients in a study prescribing placebos not meds. On days 14, 21, and 28, the doctors swabbed the patients’ noses to test the levels of viruses in the volunteers nasal secretions. At the same time, the volunteers were asked to record their symptoms.
Two weeks ago, the team published a “preprint” of the results. Full disclosure: That means they released research findings that have not yet been peer-reviewed and are not recommended as a guide in treating patients. But that doesn’t mean they aren’t valuable.
“Natural Part of the Disease”
After counting and analyzing the numbers twice, the researchers report that minus any meds, 12 percent of the volunteers ran into a viral rebound. Twenty-seven percent saw their symptoms improve but then recur. As expected, these events were more common among older volunteers (median age 54) than among younger ones (median age 47). The good news? Across the age groups, young and old, only 1-2 percent had both “high” viral reload and recurring symptoms.
What to make of this? According to Sean T. Liu, MD, PhD, Medical Director of the COVID Clinical Trials Unit at the Icahn School of Medicine at Mount Sinai, “This data suggests that the symptom and viral ‘rebound phenomenon’ may just be a natural part of the disease course of COVID-19 in the minority of individuals. Attempting to figure out the mechanism behind this effect is very challenging and involves research of the virus, the host, and their interactions. It’s unclear if a longer treatment period with Paxlovid would make a difference.”
That’s a question both Pfizer, which markets Paxlovid, and the medical community which prescribes it are anxious to answer. To do so, they’ll need to compare the no-med rebound stats with a second study of patients taking meds such as NIH’s ACTIV-2 Outpatient Monoclonal Antibodies and Other Therapies Trial testing multiple meds on 4,400 non-hospitalized COVID patients.
In the meantime, the best course appears to be sticking with the current protective but less-than-totally-preventive vaccines, a list that’s about to expand. Last Monday Pfizer BioNTech asked FDA to authorize the emergency use of a new booster specifically designed to target two new omicron subvariants in people 12 and older.
Boosting the booster with Doctor Mom’s certified chicken soup couldn’t hurt.